Everyone gets dry skin sometimes, but chronic conditions like hives or eczema are more than that. Have you experienced red, inflamed and itchy skin that seems to come back again and again, but you’re not sure where it came from?
You’re not alone. Hives and eczema (also known as atopic dermatitis) are common skin conditions that can repeatedly flare up, causing irritation, itchiness and discomfort. But even though they’re common, sometimes it can be hard to know what exactly is causing your symptoms.
As a nutritionist who has worked with hundreds of eczema patients over the last 20+ years, I’m here to help you get to know the difference between hives and eczema so you can understand your symptoms and find a treatment that works for your skin.
How to Tell the Difference Between Hives and Eczema
One reason people find it hard to know whether they have hives or eczema is that they have many similar symptoms. People with hives or eczema often experience red, itchy skin and inflamed rashes that can flare up unexpectedly, which can make daily life uncomfortable or even painful.
But luckily, there are some ways to tell them apart. Here are some of the key differences between hives and eczema:
Hives: Symptoms and Triggers
Also known as urticaria, hives show up suddenly in the form of raised, red or fleshy-coloured welts. Their appearance has been compared to large disk-like mosquito bites, however the bumps can change shape and move around within short periods of time. Hives can be incredibly uncomfortable, with sensations of itchiness, burning and stinging.
Usually, hives don’t stick around for long and they should go away within 24 hours. That is the main difference between hives and eczema—hives can often disappear fast. However, chronic hives can come and go for weeks or even months, if you keep exposing yourself to the triggers. Hives can be triggered by allergens or irritants, including certain foods (like shellfish, nuts and eggs), medications such as antibiotics or aspirin, stress or insect stings.
I previously had cold urticaria (hives), which is an allergy to cold weather and water. I would be covered in hives during winter or whenever I swam in cold water. My throat even swelled up when I drank ice cold water. I found a way to prevent cold urticaria, so let me know if you want my free treatment plan.
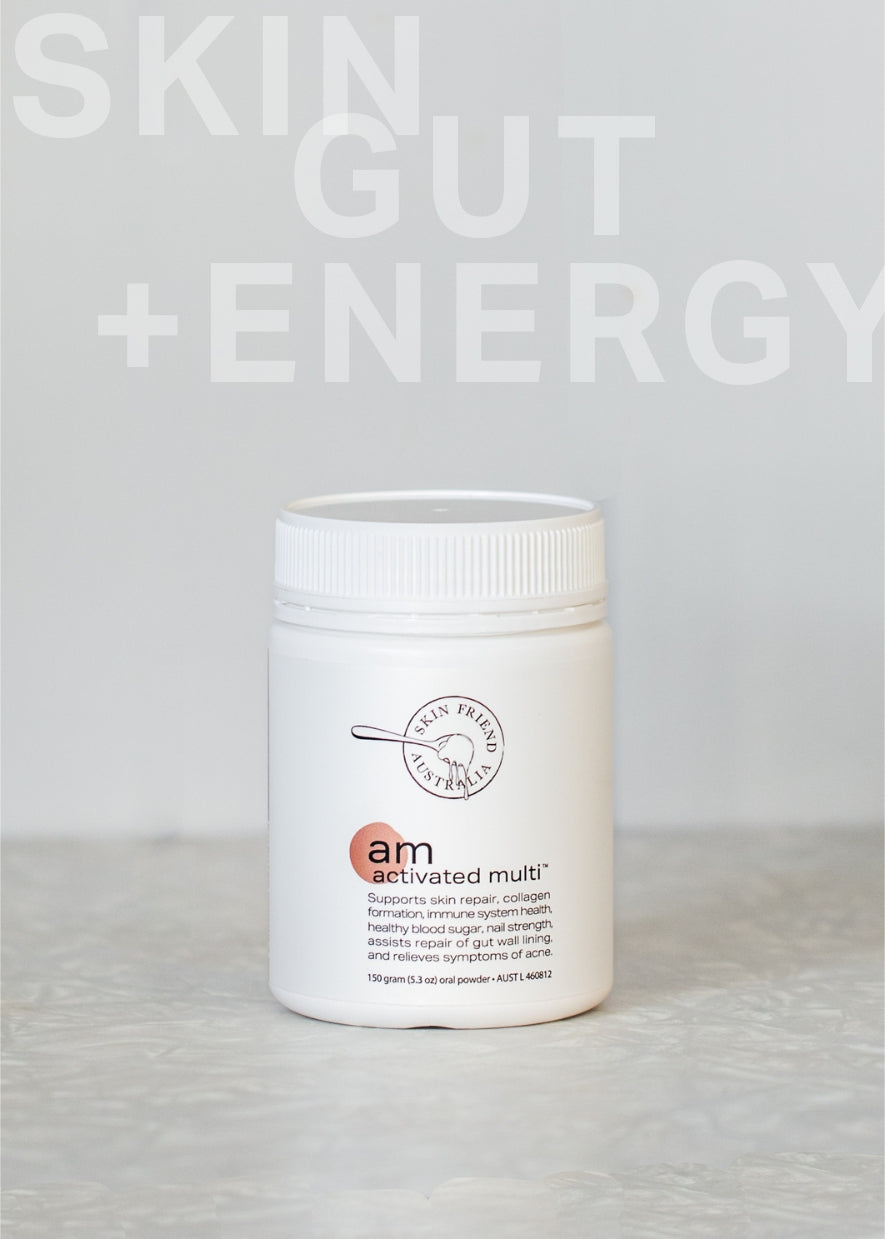
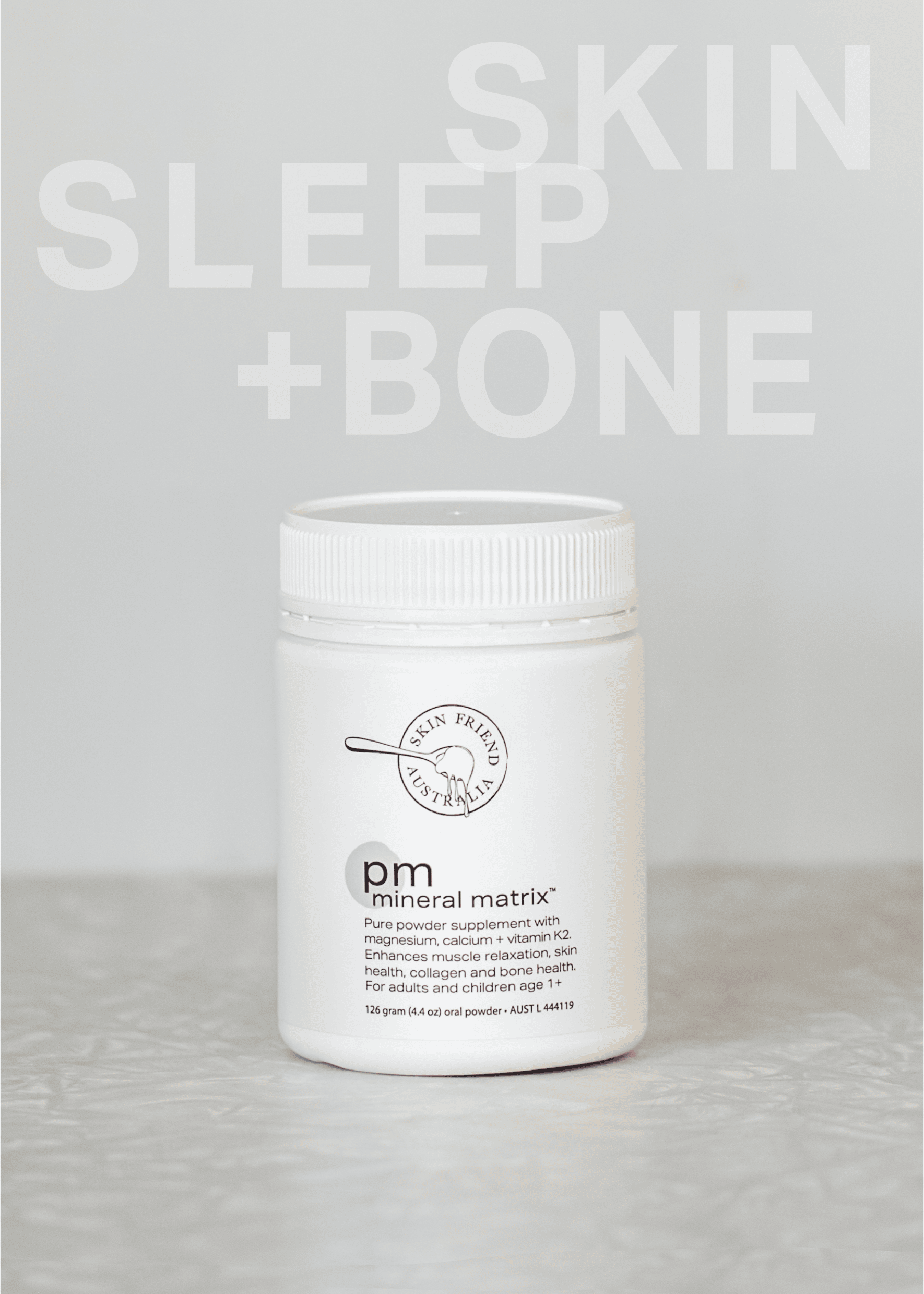
Wondering how to treat hives in adults? A good place to start is by identifying and avoiding your triggers, then supporting your body with good nutritional support and topical treatments, like Eczema Friend or Wonder Zinc. Antihistamines may be able to help short-term, but long-term relief starts with calming inflammation through natural, nutrient-rich supplements like those from Skin Friend AM and PM.
Can Salicylates Cause Hives?
Some people experience hives from food chemicals and one of the most common culprits is salicylate intolerance. Other natural chemicals that cause hives include amines and histamine, which can also trigger skin reactions in sensitive individuals. According to Dr. Anne Swain from the RPA Hospital in Sydney, food intolerance—particularly to salicylates—may be an underlying cause of chronic urticaria (long-term hives).
Low Histamine Diet for Chronic Hives: What the Science Says
Yes—scientific research shows that reducing dietary histamine may significantly improve symptoms in people with chronic hives (also known as chronic urticaria). In a clinical study, patients who followed a histamine-free diet for four weeks saw a meaningful drop in their symptom scores, even while continuing antihistamine medication. Researchers found that both the severity and activity of hives improved, with statistically significant reductions in itching and wheals. The study suggests that histamine from food may worsen symptoms in some individuals, possibly due to impaired gut barrier function caused by poor diet. For many, a low-histamine diet can ease symptoms and improve their quality of life.

Eczema: Symptoms and Triggers
Eczema (also called atopic dermatitis) is a chronic condition with periods or remission and relapse, that shows up as dry, scaly rash, weeping and oozing and intense itch. The inflamed patches of skin are often around areas such as elbows, knees, neck or hands but eczema can appear anywhere on your body. The itching sensation can be incredibly painful and may get worse during the night—but this can often be alleviated with intake of calcium and magnesium in the afternoon or before bed. Dietary changes are often required to find lasting relief from chronic eczema.
Unlike hives, eczema tends to stick around longer and may cause your skin to become thickened and cracked over time. Common triggers for eczema can include dry skin and weather changes, harsh soaps or skincare products, allergens or even stress and food allergies and intolerances, including histamine intolerance and salicylate intolerance. It has that in common with hives!
Check out our blogs to learn more about the difference between eczema vs psoriasis.
Symptom Tracking for Hives or Eczema
Learning the difference between hives and eczema can seem overwhelming at first, but you can start to recognise their differences by paying attention to the appearance of your symptoms, how long they last and what triggers your flare-ups.
Keeping a diary of your symptoms, diet and reactions is a great way to get to know what may be triggering your hives or eczema flare-ups. This information will help you manage your symptoms as you start to understand the food allergens, cosmetic products or medications which cause hives or eczema to flare.
The Gut-Skin Connection: What Causes Eczema and Hives?
While hives and eczema have various triggers, researchers believe they may be linked to immune system dysfunction, inflammation, and “leaky gut” a compromised gut lining and microbiome.
Damage to the gut lining, also known as leaky gut, can increase systemic inflammation as toxins and undigested food pass into the bloodstream, triggering immune responses that may worsen skin symptoms and contribute to flare-ups. This can also lead to deficiencies in key nutrients such as zinc and vitamin K2, which are linked to poor gut integrity and skin barrier function.
Find Relief with Skin Friend
If you’re wondering how to treat hives in adults or find relief from eczema, topical treatments and nutrient focused solutions, including a diet low in histamines and salicylates, may help to soothe your skin, repair your gut wall and reduce inflammation.
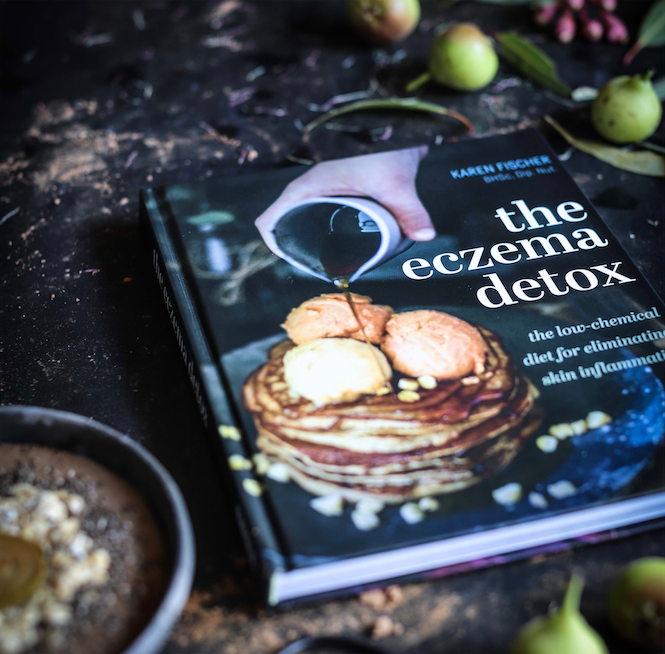
Following a low salicylate and low histamine diet can help reduce symptoms of hives and eczema by reducing gut irritants and supporting microbiome health with prebiotic fibre and specific skin nutrients. Helpful resources include The Eczema Detox and The Healthy Skin Kitchen by eczema researcher Karen Fischer, our Skin Friend founder, which offer practical guidance on avoiding histamine and salicylate-rich foods and supporting skin health from within.
Skin Friend supports gut and skin health through a science-backed approach that focuses on restoring skin strength and gut health, not masking symptoms. Our formulas are developed by a clinical nutritionist and made with targeted nutrients like zinc to support wound healing and repair of the gut wall lining, while vitamin K2 helps to protect your gut microbiome.
Ready to support your gut and calm your skin? Explore our eczema-friendly skincare and supplements and take the first step toward clearer, calmer skin from the inside out.
Click for references
Fischer K, Jones M, O’Neill HM. Prevalence of Intolerance to Amines and Salicylates in Individuals with Atopic Dermatitis: A Systematic Review and Meta-Analysis. Nutrients. 2025; 17(10):1628. https://doi.org/10.3390/nu17101628
Vanessa L. Diaz, K. et al. Cold Urticaria Syndromes: Diagnosis and Management, The Journal of Allergy and Clinical Immunology: In Practice, Volume 11, Issue 8, 2023.
Swain, A, 1988, The Role Of Natural Salicylates In Food Intolerance, retrieved 30 May 2025 from https://www.slhd.nsw.gov.au/rpa/allergy/resources/foodintol/development.html
Son JH, Chung BY, Kim HO, Park CW. A Histamine-Free Diet Is Helpful for Treatment of Adult Patients with Chronic Spontaneous Urticaria. Ann Dermatol. 2018 Apr;30(2):164-172. doi: 10.5021/ad.2018.30.2.164. PMID: 29606813; PMCID: PMC5839887.
Kim JE, Kim HS. Microbiome of the Skin and Gut in Atopic Dermatitis (AD): Understanding the Pathophysiology and Finding Novel Management Strategies. J Clin Med. 2019 Apr 2;8(4):444. doi: 10.3390/jcm8040444. PMID: 30987008; PMCID: PMC6518061.
Shahnawaz M. et al., Atopic dermatitis: Pathophysiology, microbiota, and metabolome – A Comprehensive Review, Microbiological Research, Volume 281, 2024.
Cai R, Zhou C, Tang R, Meng Y, Zeng J, Li Y, Wen X. Current insights on gut microbiome and chronic urticaria: progress in the pathogenesis and opportunities for novel therapeutic approaches. Gut Microbes. 2024.