Atopic dermatitis, also known as eczema, is one of the most common chronic skin conditions worldwide. But despite being so common, many people struggle to understand what triggers their flare-ups or how to manage symptoms effectively without relying solely on medications.
The good news is there are science-backed ways to support your skin. Research shows that lifestyle changes, gut health support, targeted nutrition, and topical atopic dermatitis treatment creams can significantly reduce inflammation and improve your skin barrier.
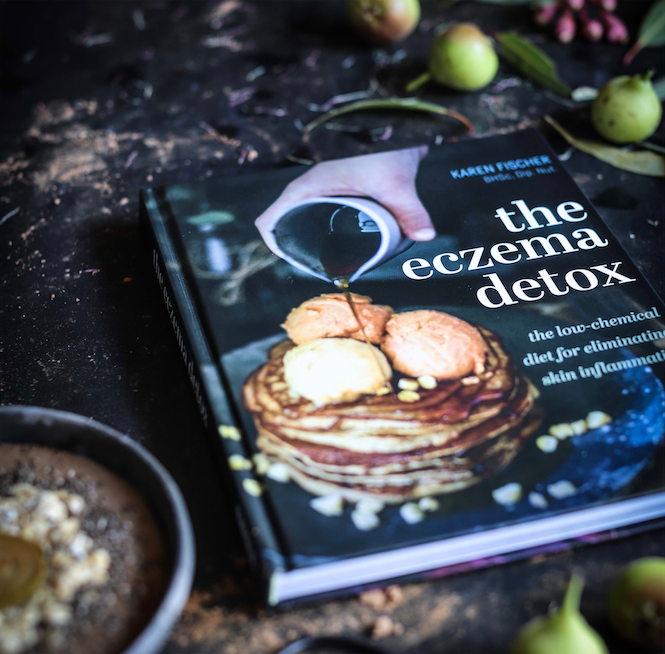
In this complete guide, we’ll explore the causes and symptoms of atopic dermatitis (including my published research on eczema and food intolerance), the difference between hives vs eczema, plus natural atopic dermatitis barrier creams and skincare tips to help you find relief.

Images: My skin when I had atopic dermatitis; close up of legs with infected atopic dermatitis; after successful natural treatments using Skin Friend and The Eczema Detox.
What is Atopic Dermatitis?
Most people think atopic dermatitis is a type of eczema but this is incorrect. Atopic dermatitis is eczema, and is now considered the accepted medical term because “atopic” means linked to allergies and “dermatitis” refers to skin inflammation.
It’s a chronic inflammatory skin condition that causes red, dry and itchy rashes. In my clinical experience with eczema, I’ve noted that food intolerance, specifically when you eat a food that irritates your eczema, can cause weeping and oozing eczema.
Atopic dermatitis often begins in infancy or early childhood, but for many, it can persist well into adulthood. Eczema affects around 225 million people (Arents, 2023), making it one of the most widespread skin disorders.
Causes:
While there is no single cause of eczema, researchers agree that it’s linked to a combination of health, environmental and genetic factors. Common causes include:
- Weakened or damaged skin barrier.
- Genetics (can be associated with other atopic conditions like asthma and hay fever).
- Immune dysfunction and overactive immune responses.
- Environmental triggers such as weather changes, pollution, allergens and harsh skincare products.
-
Histamine intolerance and salicylate intolerance.
-
Food allergies and sensitivities to common foods including dairy, eggs, wheat, peanut and soy.
- Deficient diets that are particularly low in zinc and calcium.
Symptoms:
- Red, itchy, inflamed rashes and chronically dry, cracked skin.
- May develop infections, blisters, oozing and crusting.
- For many people, itchiness gets worse at night—or after eating foods they’re allergic or sensitive to, which can trigger flares.
- Skin sensitivity to irritants such as fragrances, PFAS (forever chemicals found in skincare products and fabrics), soaps, wool or sweat.
- Can appear anywhere on the body, but is common on the hands, face, neck, elbows and knees.
Atopic Dermatitis vs Hives: What’s the Difference?
While both atopic dermatitis (eczema) and hives (urticaria) involve red, itchy skin, they are very different conditions, with their own distinct causes, symptoms and treatment approaches.
Hives are characterised by a flare-up of red bumps that have a burning and stinging sensation. However, they tend to appear on a more temporary basis. Both hives and eczema can be symptoms of immune dysregulation, and intolerance to dietary salicylates and histamine, and may benefit from gut health support and nutrient therapy, especially if they’re recurring or difficult to manage.
Understanding the difference between atopic dermatitis vs hives is key to managing your skin effectively and choosing the right care. If you’re experiencing regular flare-ups of either condition, tracking your symptoms and triggers, including diet and lifestyle, can be a helpful first step toward relief.
Managing Eczema: Atopic Dermatitis Treatment Creams and Skincare Tips
When it comes to managing eczema, having a gentle skincare routine can help you alleviate the dryness and itchiness that often come with the condition. Here are some daily skincare tips for eczema-prone skin:
- Moisturise morning and night with an atopic treatment barrier cream, such as Eczema Friend, which is steroid-free and certified PFAS-free.
- Use lukewarm water only, hot showers can worsen dryness and inflammation.
- Choose soft, breathable fabrics like cotton; avoid wool or synthetic fibres.
- Patch test new skincare products before applying them to large areas.
- Avoid harsh soaps – use pH-balanced, fragrance-free cleansers instead.

Do eczema creams work better after a shower—or on dry skin?
It’s a common myth that skin creams should be applied immediately after bathing to lock in moisture while the skin is slightly damp. In contrast, a study on people with eczema found they’re more effective when applied to dry skin. Here’s what they discovered:
- You should apply moisturiser after bathing because it reduces skin hydration.
- Applying moisturiser after showering improved skin hydration only modestly.
- The greatest hydration benefit came from applying cream to dry skin—especially 30 minutes (or longer) after bathing.
Why dry skin? Because water repels the oils and actives in skincare (water and oils don’t mix!), making it harder for creams to absorb and provide long-lasting relief. If you’ve just showered, it’s beneficial to moisturise—but if you have eczema, reapplying the cream to dry skin later can offer deeper, longer-lasting hydration.
Managing eczema isn’t just about calming flare-ups or “getting through the day”. It’s about supporting your skin long-term with ingredients that restore, protect, and nourish the skin barrier. Conventional treatments that rely on corticosteroids, which may provide temporary relief, can weaken the skin over time.
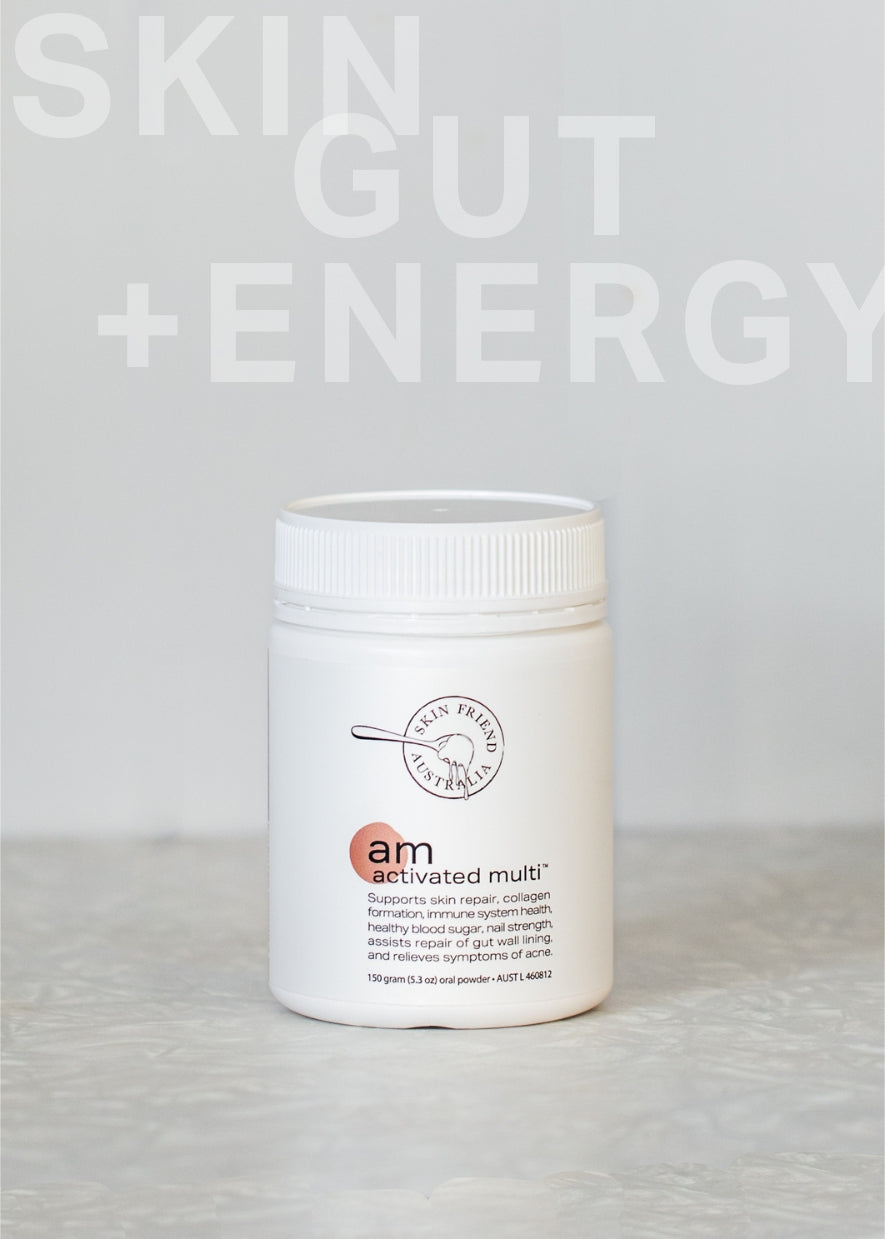
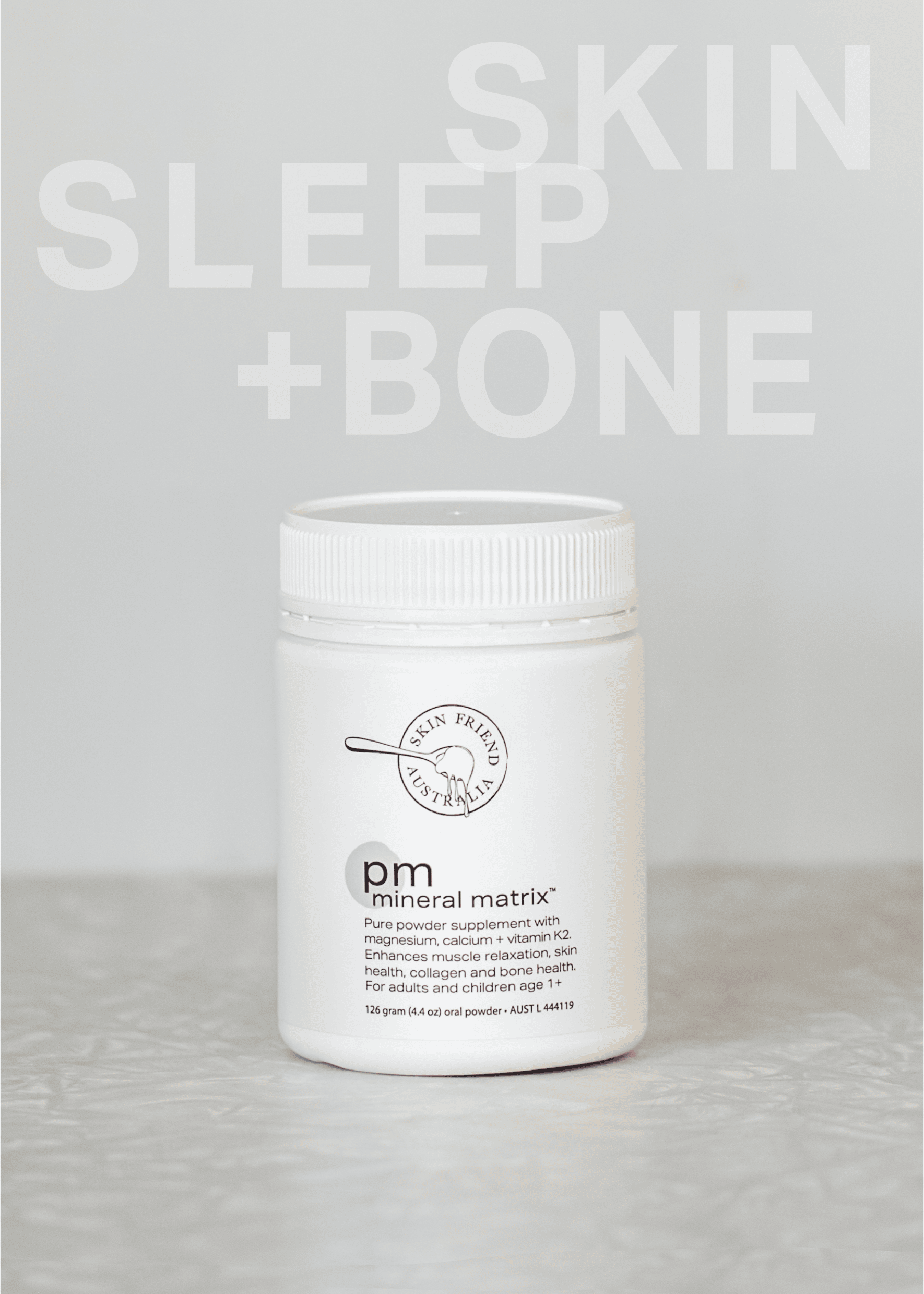
At Skin Friend, we focus on drug-free, nutrient-based skincare that’s gentle on sensitive skin and designed to work in harmony with your body’s natural healing process. Our atopic dermatitis treatment creams are fragrance free and non-toxic while rich in skin-supporting ingredients, including organic seaweed extract to reduce the appearance of red skin and support the skin microbiome and provitamin B5 to repair the skin barrier and relieve itchy skin.
Discover Skin Friend’s Atopic Dermatitis Barrier Creams
Eczema skincare isn’t one-size-fits-all. It’s about consistent, gentle care that supports the skin barrier and reduces inflammation over time. And while topical treatments like atopic dermatitis barrier creams are an important first step, it’s also important to support your skin from within using targeted gut-support treatments and nutrients.
With eczema skincare and supplements from Skin Friend, you’ll find soothing treatments that are non-toxic, and full of nourishing ingredients like provitamin B5 and organic seaweed extract. By taking the steps to support your skin within and without, you’ll be able to calm your eczema while supporting your overall wellbeing and helping to prevent flare ups from occurring.
Click for references
Fischer, Karen, Mark Jones, and Hayley M. O’Neill. 2025. "Prevalence of Intolerance to Amines and Salicylates in Individuals with Atopic Dermatitis: A Systematic Review and Meta-Analysis" Nutrients 17, no. 10: 1628. https://doi.org/10.3390/nu17101628
Arents BWM, van Zuuren EJ, Hughes O, Fedorowicz Z, Flohr C. The future is now: the Global Atopic Dermatitis Atlas (GADA). Br J Dermatol. 2023 Nov 16;189(6):761-763. doi: 10.1093/bjd/ljad286. PMID: 37566747.
Christensen MO, et al. Prevalence of and association between atopic dermatitis and food sensitivity, food allergy and challenge-proven food allergy: A systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2023 May;37(5):984-1003. doi: 10.1111/jdv.18919. Epub 2023 Feb 8. PMID: 36695076.
Peroni DG, Hufnagl K, Comberiati P, Roth-Walter F. Lack of iron, zinc, and vitamins as a contributor to the etiology of atopic diseases. Front Nutr. 2023 Jan 9;9:1032481. doi: 10.3389/fnut.2022.1032481. PMID: 36698466; PMCID: PMC9869175.
Vaughn AR, Foolad N, Maarouf M, Tran KA, Shi VY. Micronutrients in Atopic Dermatitis: A Systematic Review. J Altern Complement Med. 2019 Jun;25(6):567-577. doi: 10.1089/acm.2018.0363. Epub 2019 Mar 26. PMID: 30912673.
Maywald M, Rink L. Zinc Deficiency and Zinc Supplementation in Allergic Diseases. Biomolecules. 2024; 14(7):863. https://doi.org/10.3390/biom14070863
Hildebrand H, Simons E, Kozyrskyj AL, Becker AB, Protudjer JL. Calcium Intake in Children with Eczema and/or Food Allergy: A Prospective Cohort Study. Nutrients. 2019 Dec 12;11(12):3039. doi: 10.3390/nu11123039. PMID: 31842448; PMCID: PMC6950300.